-
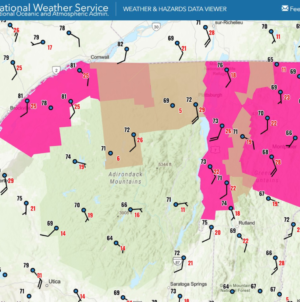
Red Flag Warnings Issued in These States: What To Know - 17 mins ago
-
Sam Rivers, Bassist for Limp Bizkit, Dies at 48 - 19 mins ago
-
Healthcare workers strike at Kaiser Permanente ends after 5 days - 23 mins ago
-
Panthers’ Bryce Young Exits Game With Worrisome Ankle Injury - 54 mins ago
-
U.S. Kills 3 on Boat Suspected of Smuggling Drugs for Colombian Rebels - about 1 hour ago
-
College Football Program Fires Coach After 12-Point Loss - about 1 hour ago
-
A Fragile Cease-fire Between Afghanistan and Pakistan Ends Violence, for Now - 2 hours ago
-
Dodgers’ Mookie Betts Sends Message to Brewers After NLCS - 2 hours ago
-
Epoch Times Reporter Resigns After Publication Signs Pentagon Rules - 3 hours ago
-
Florida Fires Billy Napier After Two-Point Win - 3 hours ago
Up to 70% of American Adults Could Be Obese With ‘More Accurate’ Definition
Nearly 70 percent of American adults could be classified as obese under an updated definition that factors in more than just body mass index (BMI).
This is the finding of Harvard University researchers who—following a Lancet Commission proposing the new definition back in January—investigated what the implications of adopting such would be.
Their analysis of more than 300,000 Americans from the All of Us Research Program—a large, nationally representative U.S.-based cohort—found that the prevalence of obesity in the U.S. rose to 68.6 percent, a 60 percent increase from the current number.
BMI has long been seen by some as an outdated tool, with the new definition potentially “more accurate,” according to experts.
“The key takeaway is we’re really trying to look at what obesity means and address those individuals who are clinically obese and would be considered so by using more than just criteria as defined by BMI,” said Dr. Armando Castro-Tie, chair of surgery at South Shore University Hospital Northwell Health, who wasn’t involved in the research, in a statement.

“Traditionally, obesity has been defined by a high BMI, where BMI reflects weight relative to height. However, BMI is an imprecise measure of body composition as it does not distinguish between fat and muscle or indicate fat distribution,” study author and endocrinologist professor Lindsay T. Fourman of Harvard Medical School told Newsweek.
“For example, athletes may have a high BMI due to greater muscle mass rather than excess fat, while others may have normal BMI but carry excess abdominal fat that increases metabolic risk.
“The new Lancet definition goes beyond BMI to better capture body composition by incorporating anthropometric measurements [measurements of the human body] like waist circumference or waist-hip ratio that can be easily obtained in a doctor’s office.”
Fourman explained that, under the new definition, someone is classified as having obesity if they have either an elevated BMI plus at least one elevated anthropometric measure, or elevated anthropometric measures despite a normal BMI.
“The latter group—which we term ‘anthropometric-only obesity’—represents a major paradigm shift, recognizing that even individuals with normal weight may face obesity-related health risks if they have excess abdominal fat,” she added.
The rise detected was driven by this inclusion of anthropometric-only obesity, while the guidelines also identify and distinguish between when obesity is a risk factor (preclinical obesity) and when it represents a stand-alone illness (clinical obesity).
“Our findings support the updated definition, demonstrating that people with anthropometric-only obesity are at increased health risk,” said Fourman.
“One area where our findings may differ from the guidelines concerns preclinical obesity. The guidelines suggest lower urgency and intensity of care for preclinical obesity, reserving pharmacologic and surgical interventions for select cases.
“Our data indicate that people with preclinical obesity are still at higher long-term risk of health complications compared to those without obesity. Additionally, clinical obesity prevalence increased with age, suggesting that preclinical obesity may progress to clinical obesity over time.”
Fourman also emphasized it turns out people may not have been overclassified as much as previously thought by the traditional definition of obesity. “Almost everyone with obesity by the traditional BMI-based definition still meets criteria when the additional requirement of an elevated anthropometric measure is applied.”
Castro agrees with adopting the guidelines, saying: “As it is, even with the current definitions, we know that number one: there’s a lot of stigma around it. More importantly, the lack of really being more inclusive of what obesity looks like in our population.”
“It doesn’t allow or doesn’t afford individuals with the care that we know can be of benefit to them in terms of addressing the issues of being overweight or being obese, certain medications, certain access to different kinds of treatment, things like that. “
Castro acknowledged people may be skeptical about perceived intentions to monopolize on obesity treatments and make more money.
“I think that it’s short sighted, and at the end of the day, we know that we have treatments and modalities that are of clinical benefit to patients who are suffering from obesity. It is our duty to make sure that we are identifying who these individuals are in an unbiased and in a scientifically rigorous way to make sure that we are affording everybody who fits these criteria.”
He added the new criteria “now forces us as clinicians to really think about what is appropriate for what level of obesity in a more thoughtful and intentional way.”
The study authors acknowledged, however, that their findings also highlight critical gaps in knowledge in terms of anthropometric-only obesity, preclinical obesity and the “shifting target population for obesity pharmacotherapy”—with more research needed to inform evidence-based care of these groups.
Do you have a tip on a health story that Newsweek should be covering? Do you have a question about obesity? Let us know via health@newsweek.com.
Reference
Fourman, L. T., Awwad, A., Gutiérrez-Sacristán, A., Dash, C. A., Johnson, J. E., Thistle, A. K., Chahal, N., Stockman, S. L., Toribio, M., Anekwe, C., Gattu, A. K., & Grinspoon, S. K. (2025). Implications of a New Obesity Definition Among the All of Us Cohort. JAMA Network Open, 8(10). https://doi.org/10.1001/jamanetworkopen.2025.37619
Rubino, F., Cummings, D. E., Eckel, R. H., Cohen, R. V., Wilding, J. P. H., Brown, W. A., Stanford, F. C., Batterham, R. L., Farooqi, I. S., Farpour-Lambert, N. J., Roux, C. W. le, Sattar, N., Baur, L. A., Morrison, K. M., Misra, A., Kadowaki, T., Tham, K. W., Sumithran, P., Garvey, W. T., … Mingrone, G. (2025). Definition and diagnostic criteria of clinical obesity. The Lancet Diabetes & Endocrinology, 13(3), 221–262. https://doi.org/10.1016/S2213-8587(24)00316-4
Source link